
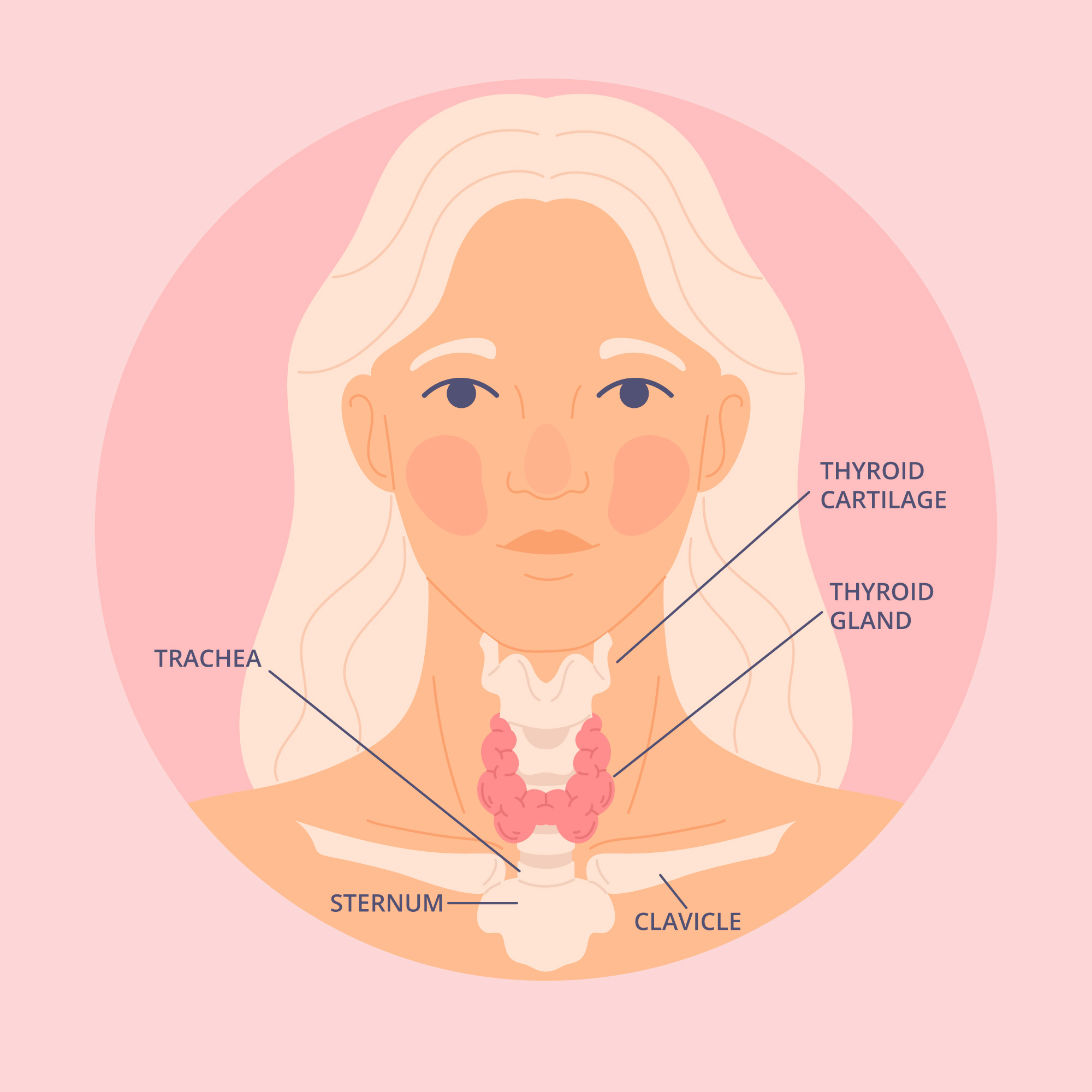
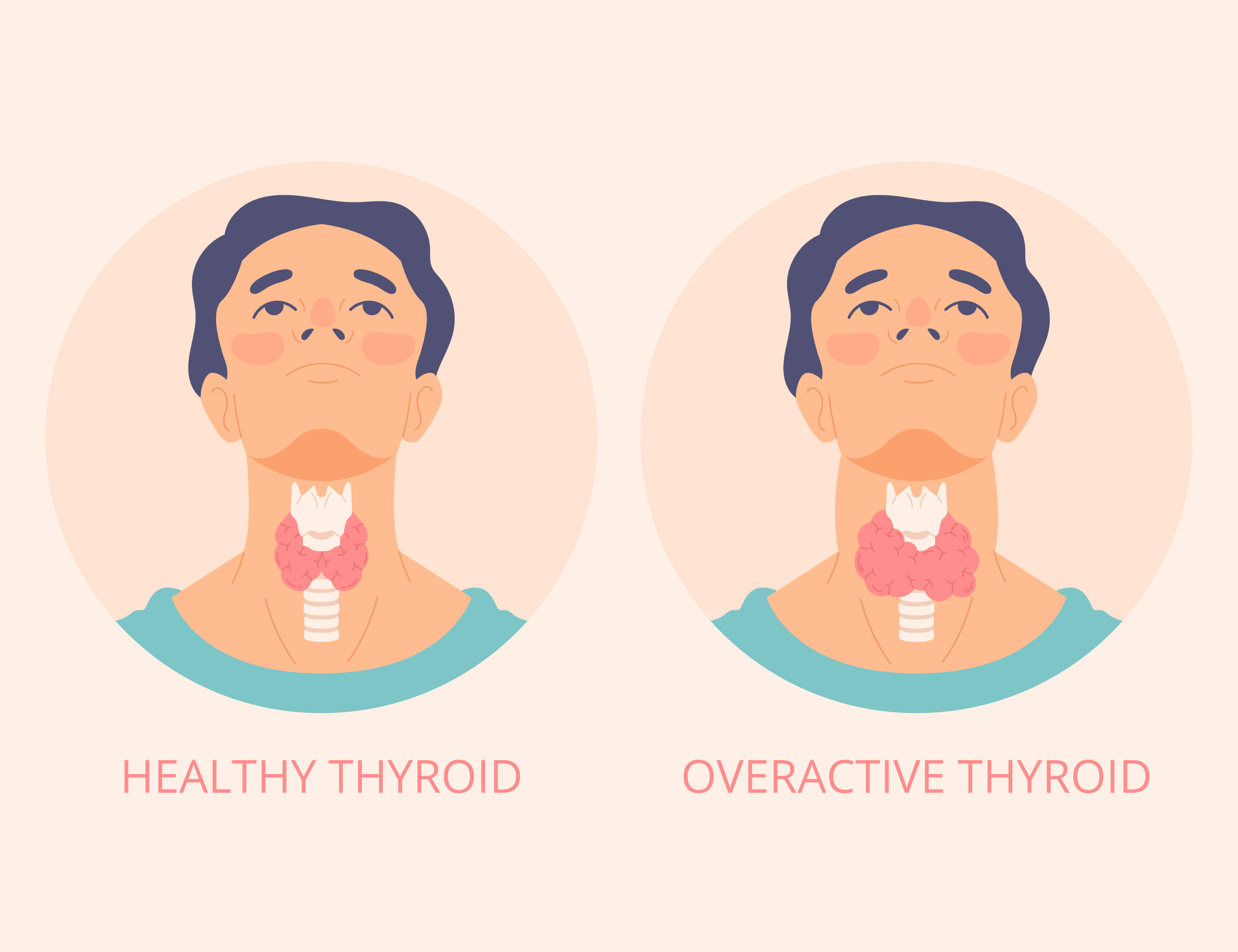
Thyroid cancer is a type of cancer that originates in the thyroid gland, a butterfly-shaped gland located at the base of the neck. The thyroid gland produces hormones that regulate metabolism, heart rate, and body temperature. There are several types of thyroid cancer, each with different characteristics, treatments, and prognoses.
Treatment
1. Surgery
Thyroidectomy : Partial or total removal of the thyroid gland.
Lymph Node Removal : If cancer has spread to nearby lymph nodes.
2. Radioactive Iodine Therapy
Used to destroy remaining cancerous thyroid tissue post-surgery.
3. Thyroid Hormone Therapy
Suppresses the production of thyroid-stimulating hormone (TSH), which can promote cancer growth.
4. External Radiation Therapy
Used for more advanced cancers that do not respond to radioactive iodine therapy.
5. Chemotherapy
Typically used for anaplastic thyroid cancer or other advanced cancers.
6. Targeted Therapy
Drugs that target specific genetic mutations in cancer cells.
Prognosis
The prognosis for thyroid cancer varies based on the type and stage at diagnosis. Generally, papillary and follicular thyroid cancers have excellent survival rates, particularly when detected early. Medullary thyroid cancer prognosis depends on whether it is sporadic or familial and the extent of the disease. Anaplastic thyroid cancer has a poor prognosis due to its aggressive nature.
Follow-Up Care
• Regular monitoring through physical exams, blood tests, and imaging studies.
• Lifelong thyroid hormone replacement therapy if the thyroid is removed.
Prevention and Early Detection
• Regular check-ups for individuals at high risk (e.g., those with a family history or past radiation exposure).
• Awareness of symptoms and seeking medical advice if any signs are noticed.
Early detection and appropriate treatment are crucial in managing thyroid cancer effectively and improving outcomes.